Prevent and Treat Peptic Ulcer Disease Naturally

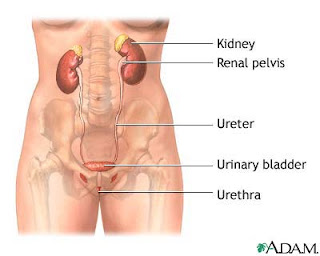
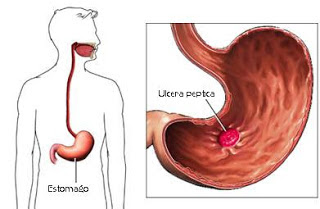
Peptic Ulcer Disease is the most common ulcer of an area of the gastrointestinal tract that is usually acidic and thus extremely painful. Four times as many peptic ulcers arise in the duodenum—the first part of the small intestine, just after the stomach—as in the stomach itself.
The main symptom of peptic ulcer is upper abdominal pain which can be dull, sharp, or burning. (Bloating and burping are not symptoms of peptic ulcer, and vomiting, poor appetite, and nausea are uncommon symptoms of peptic ulcer.)
Symptoms of a peptic ulcer can be :
- abdominal pain, classically epigastric strongly correlated to mealtimes. In case of duodenal ulcers the pain appears about three hours after taking a meal;
- bloating and abdominal fullness;
- waterbrash (rush of saliva after an episode of regurgitation to dilute the acid in esophagus - although this is more associated with gastroesophageal reflux disease);
- nausea, and copious vomiting;
- loss of appetite and weight loss;
- hematemesis (vomiting of blood); this can occur due to bleeding directly from a gastric ulcer, or from damage to the esophagus from severe/continuing vomiting.
- melena (tarry, foul-smelling feces due to oxidized iron from hemoglobin);
- rarely, an ulcer can lead to a gastric or duodenal perforation, which leads to acute peritonitis. This is extremely painful and requires immediate surgery.
Prevent and Treat Peptic Ulcer Disease Naturally
The best efforts to prevent ulcer disease is to eat on time, that is regular and not excessive, a balanced lifestyle and healthy, hygiene, and avoid stress.
As for treating ulcer disease can naturally use the following herbal ingredients:
The first drug ulcer disease (Avocado)
Ulcer disease, the first drug that is using avocado fruit seeds. To make it, wash the avocado seed, with boiled water, then grated avocado seed and mix 100 cc of boiled water with grated avocado seed before, then strain.
Rules used ulcer drugs:
mild ulcer disease, drinking juice avocado seeds 1 a day;
Chronic ulcer disease, drinking juice avocado seed 2 times a day, morning and evening, until healed.
The second drug ulcer disease (Turmeric)
The second ulcer drug use turmeric herb. To make it, take 2 segment turmeric, then peeled and cleaned, then grated turmeric, add boiled water, and squeeze to take out the juice.
For rules of use, drink twice a day, in the morning before eating and at night before bed.
That prescription natural remedy to overcome ulcer disease, which is down termurun been handed down by our ancestors. Hopefully ulcer disease herbal medicine can help those of you who are experiencing ulcer disease, whether mild, moderate or chronic.













.jpg)


