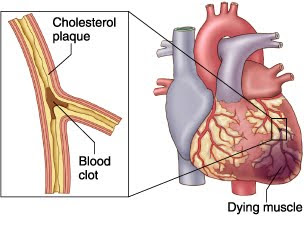
Acute Pain related to Myocardial Infarction
Nursing Diagnosis : Acute Pain related to Myocardial Infarction
Goals and Expected outcomes :
The expected outcomes:
Nursing Interventions - Acute Pain related to Myocardial Infarction
Independent
1. Monitor or record the characteristics of the pain, noted the report verbal, nonverbal cues, and the haemodynamic response (grimacing, crying, anxiety, sweating, clutching his chest, rapid breathing, blood pressure / heart frequency change).
Rational: Variations in the appearance and behavior of the patient as pain occurs as the assessment findings. Most patients with Acute Myocardial Infarction looks sick, distraction, and focus on the pain. History of verbal and deeper investigation of the precipitating factors should be delayed until the pain is gone. Breathing may be increased as a result of pain and is associated with anxiety, stress cause temporary loss of catecholamines would increase heart rate and blood pressure.
2. Take a complete picture of the pain of the patient, including the location, intensity (0-10), duration, quality (shallow / spread), and distribution.
Rational:
Pain is a subjective experience and should be described by the patient. Help patients to assess pain by comparing the experience of others.
3. Observations over the previous history of angina, pain resembling angina, or pain in Myocardial Infarction. Discuss family history.
Rational:
Can compare the pain is there from the previous pattern, according to the identification of complications such as widespread infarction, pulmonary embolism, or pericarditis.
4. Instruct patient to report pain immediately.
Rational:
Delays in the reporting of pain, inhibit pain relief and require increased doses of the drug. In addition, severe pain can cause shock by stimulating the sympathetic nervous system, resulting in further damage and interfere with diagnostic and pain relief.
5. Provide a quiet, slow activity, and comfortable action (eg, bed linen dry / not crossed, rubbing his back). Patient approach calmly and with confidence.
Rational:
Lowering external stimuli in which anxiety and heart strain and limited coping abilities and judgment of the current situation.
6. Assist patients in relaxation techniques, eg, deep breathing / slow, behavioral distraction, visualization, imagination guidance.
Rational:
Assist in the reduction in the perception / response to pain. Giving control of the situation, increase positive behavior.
7. Check vital signs before and after drug pemnerian.
Rational:
Hypotension / respiratory depression can occur as a result of the provision. This problem can increase the myocardial damage in the presence of ventricular failure.
Collaboration:
8. Give supplemental oxygen by nasal cannula or mask as indicated.
rational:
Increasing the amount of oxygen available for myocardial usage and also reduce discomfort in relation to tissue ischemia.
Goals and Expected outcomes :
- Expected loss or uncontrolled chest pain
The expected outcomes:
- Patients are able to demonstrate the use of relaxation techniques.
- Patients showed reduced stress, relaxed and easy to move.
Nursing Interventions - Acute Pain related to Myocardial Infarction
Independent
1. Monitor or record the characteristics of the pain, noted the report verbal, nonverbal cues, and the haemodynamic response (grimacing, crying, anxiety, sweating, clutching his chest, rapid breathing, blood pressure / heart frequency change).
Rational: Variations in the appearance and behavior of the patient as pain occurs as the assessment findings. Most patients with Acute Myocardial Infarction looks sick, distraction, and focus on the pain. History of verbal and deeper investigation of the precipitating factors should be delayed until the pain is gone. Breathing may be increased as a result of pain and is associated with anxiety, stress cause temporary loss of catecholamines would increase heart rate and blood pressure.
2. Take a complete picture of the pain of the patient, including the location, intensity (0-10), duration, quality (shallow / spread), and distribution.
Rational:
Pain is a subjective experience and should be described by the patient. Help patients to assess pain by comparing the experience of others.
3. Observations over the previous history of angina, pain resembling angina, or pain in Myocardial Infarction. Discuss family history.
Rational:
Can compare the pain is there from the previous pattern, according to the identification of complications such as widespread infarction, pulmonary embolism, or pericarditis.
4. Instruct patient to report pain immediately.
Rational:
Delays in the reporting of pain, inhibit pain relief and require increased doses of the drug. In addition, severe pain can cause shock by stimulating the sympathetic nervous system, resulting in further damage and interfere with diagnostic and pain relief.
5. Provide a quiet, slow activity, and comfortable action (eg, bed linen dry / not crossed, rubbing his back). Patient approach calmly and with confidence.
Rational:
Lowering external stimuli in which anxiety and heart strain and limited coping abilities and judgment of the current situation.
6. Assist patients in relaxation techniques, eg, deep breathing / slow, behavioral distraction, visualization, imagination guidance.
Rational:
Assist in the reduction in the perception / response to pain. Giving control of the situation, increase positive behavior.
7. Check vital signs before and after drug pemnerian.
Rational:
Hypotension / respiratory depression can occur as a result of the provision. This problem can increase the myocardial damage in the presence of ventricular failure.
Collaboration:
8. Give supplemental oxygen by nasal cannula or mask as indicated.
rational:
Increasing the amount of oxygen available for myocardial usage and also reduce discomfort in relation to tissue ischemia.